Introduction: A growing body of evidence has confirmed the association between monoclonal gammopathy of undetermined significance (MGUS) and a variety of diseases including bone disease, renal impairment, autoimmune disorders, neuropathies, secondary immunodeficiencies, and infections. Recently, there has been an emerging focus on cardiovascular (CV) outcomes in patients with MGUS. However, they have not been investigated well, especially among hospitalized patients. In our study, we investigated the association between MGUS and cardiovascular outcomes in a hospital setting using the National Inpatient Sample database.
Methods: MGUS patients were sampled using ICD-10 codes. Patients less than the age of 18 years, those with missing data, and those with concomitant multiple myeloma, smoldering multiple myeloma, B-cell lymphomas, non-Hodgkin lymphomas, amyloidosis, and Waldenstrom's macroglobulinemia were excluded . Patients were stratified into two cohorts based on the presence or absence of MGUS. Comorbidities and CV outcomes were collected using ICD 10 DM codes. CV outcomes were evaluated before and after 1:1 matching for age, gender, and race. Furthermore, a sensitivity analysis was performed where all individuals with a history of diabetes mellitus (DM), prior myocardial infarction, hypertension, chronic kidney disease (CKD) stage 3-5, dialysis-dependence, obesity, metabolic syndrome, cancer (all-cause), antiplatelet or oral anticoagulant use were excluded. CV outcomes were then reevaluated using multivariate logistic regression to adjust for smoking, dyslipidemia, and aspirin use. P-values < 0.05 was considered statistically significant.
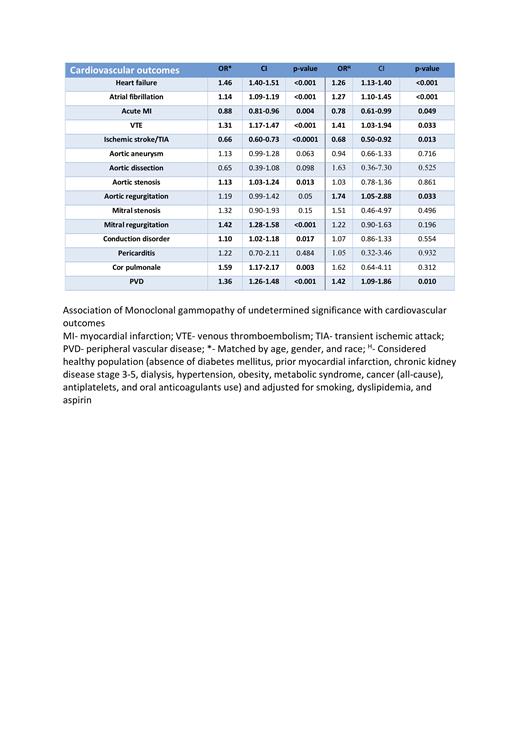
Results: Out of a total of 17,357,556 patients included in the study, 23,435 patients had MGUS (0.1%). MGUS patients tended to be older, male, smokers, and Caucasian. Additionally, MGUS patients tended to have more DM (39.2% vs 27.9%), CKD (33.6% vs 8.6%), dialysis-dependence (13.3% vs 4%), obesity (18% vs 16.5%), dyslipidemia (39.1% vs 23.3%), metabolic syndrome (18.9% vs 10.4%), and cancer (12.9% vs 8.1%) when compared to non-MGUS patients. Aspirin, antiplatelets, and anticoagulant use were more prevalent in the MGUS patients when compared to non-MGUS patients. MGUS patients had more heart failure (36.8% vs 17.2%;p<0.001), atrial fibrillation (10% vs 5.9%;p<0.001), venous thromboembolism (VTE) (2.8% vs 1.6%;p<0.001), aortic aneurysm (2.2% vs 1%;p=0.005), aortic stenosis (4.0% vs 1.6%;p<0.001), aortic regurgitation (1.2% vs 0.5%;p<0.001), mitral stenosis (0.3% vs 0.1%;p=0.009), mitral regurgitation (3.5% vs 1.5%;p<0.001), conduction disorder (6.6% vs 3.3%;p=0.002), cor-pulmonale (0.4% vs 0.2%;p<0.001), peripheral vascular disease (PVD) (14.4% vs 5.6%;p<0.001), and acute myocardial infarction (MI) (4.5% vs 3.6%;p<0.001). There were no significant differences in ischemic stroke/transient ischemic attack (TIA) and aortic dissection rates among both groups. The matched model corroborated several of our unmatched findings that MGUS was associated with higher heart failure, atrial fibrillation, VTE, aortic stenosis, mitral regurgitation, conduction disorder, cor-pulmonale, and PVD. Acute MI and ischemic stroke/TIA rates were negatively associated with MGUS in our matched model. Finally, sensitivity analysis showed that MGUS was still associated with higher rates of heart failure, atrial fibrillation, VTE, aortic regurgitation, and PVD, but decreased ischemic stroke/TIA and acute MI rates.
Conclusion: In conclusion, our study found that patients with MGUS are at an increased risk of a wide spectrum of cardiovascular diseases in a hospital setting. MGUS patients may benefit from cardiovascular screening tools like electrocardiograms and echocardiograms at the hospital as this disease is independently associated with cardiovascular outcomes. Additional studies are needed to corroborate these findings as this will have implications on monitoring and screening of cardiovascular complications in MGUS patients.
Disclosures
No relevant conflicts of interest to declare.